ImageGuide: A Recognized QCDR
CMS has recognized the ImageGuide Registry as a Qualified Clinical Data Registry (QCDR) since 2015. The designation as a QCDR allows physicians to meet reporting requirements under the Merit-based Incentive Payment System (MIPS), and it allows for the development of unique performance measures that capture a greater level of granularity with more meaning to the profession than traditional MIPS measures.
What is a QCDR?
As a QCDR, ImageGuide allows participating physicians to report on performance measures developed specifically for nuclear cardiology and echocardiography to satisfy reporting requirements under the Quality Category of the Merit-Based Payment System (MIPS). Successful participation in MIPS will allow physicians to avoid an automatic negative payment adjustment on Medicare receivables. Participants will also be able to attest to Improvement Activities and Advancing Care Information.
What are the benefits of participation in the Merit-Based Incentive Payment System (MIPS)?
In 2017, physicians who did not satisfactorily report data on quality measures will be subject to a 4% negative payment adjustment for all services rendered in 2019 for patients with Medicare Part B Fee for Service (FFS). In 2018, physicians who do not satisfactorily report data on quality measures will be subject to a 5% negative payment adjustment in 2019.
The negative payment adjustment continues each subsequent year in the event a physician does not satisfactorily report data on quality measures in the preceding year. Payment adjustments with the implementation of the Merit-Based Incentive Payment System (MIPS) program, under which physicians will be subject to payment adjustments based on MIPS participation by the following schedule:
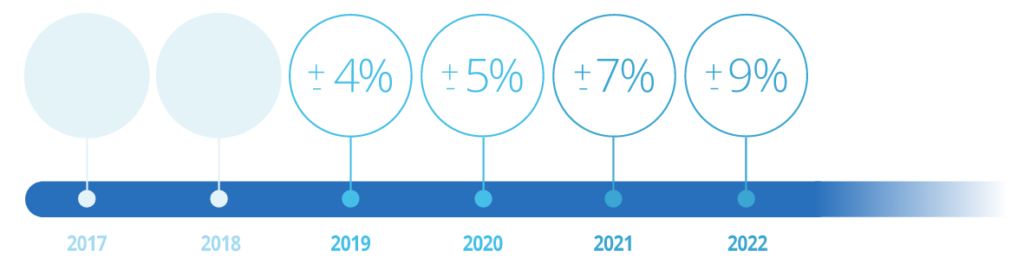
Maximum adjustment to provider's base rate of Medicare Part B payment
Will I receive a negative payment adjustment on only the imaging studies performed on patients with Medicare Part B, or does the penalty apply to all Medicare Part B services rendered?
The adjustment applies to all Medicare Part B services rendered. For example, a physician who does not successfully participate in MIPS in 2017 will be penalized 4% for all Medicare Part B services rendered in 2019.
